By David McKalip, M.D.
As President of the Florida Chapter of the AAPS, I submitted comments today to the Centers for Medicare and Medicaid Services on their proposed “MIPS” rules. MIPS (Merit-based Incentive Payment System) is an onerous command and control structure for doctors using financial and administrative penalties to coerce medical practice away from the interests of individual patients and toward the interests of government and corporate third parties. The law that allows the Obama administration to create MIPS was called MACRA (HR2) and passed last year with the full and enthusiastic support of the AMA and 49 of 50 state medical societies (only New York refused to support it).
These rules will harm patients and their doctors, placing a wedge between them that will break the most critical bond of the patient-physician relationship: trust. Patients will now wonder, “Is my doctor withholding medical care simply to obtain a government bonus?” Patients will ask, “Is my doctor giving me the best care for my individual needs in his judgment or simply following a government cookbook to serve another master?” Doctors will ultimately wonder, “Why did I try to get the bonus, instead of simply taking care of my patient?”
Excerpts of the comments are reproduced below and the full letter, with detailed references to exact rule and law language is available for download here.
Excerpts…
“Comments by Florida Chapter, Association of American Physicians and Surgeons and David McKalip, M.D., June 24, 2017 on MIPS Rules pursuant to MACRA”
“We (AAPS-FL and David McKalip, M.D.) write to point out that the proposed rules are an invalid exercise of delegated parliamentary authority. They are written in an arbitrary and capricious fashion and violate applicable administrative and other law. They are over-broad and will cause harm to physicians and their patients. These rules would cause patients harm by 1) causing physicians to alter practice patterns to satisfy the rules to achieve a bonus, avoid a penalty or avoid other harm to their practices and 2) interfering with the ability to practice medicine independently and in the best interest of their patients. The rules will cause substantial and unacceptable unfunded expenses and burdens on physician practices and deprive physicians of their time with patients since they must instead be coerced to spend time on onerous compliance activities.”
………
“(1) Mandatory Participation is unlawful.
There is a glaring and obvious violation of the law. The rule states that all MIPS eligible clinicians “MUST” (emphasis added) submit data and more.
“§ 414.1325 Data submission requirements. (a) Data submission performance categories. MIPS eligible clinicians and groups must submit measures, objectives, and activities for the quality, CPIA, and advancing care information performance categories.”
The law authorizing these rules (HR2, 114th Congress, “MACRA”) specifically denies the ability of any agency of the government to require submission of any data under MIPS. Title I, Section 101 indicates that participation in the MIPS program is completely voluntary. Page 41 of HR2 (as published by the GPO) indicates that Title I, Section 101, (c)(1)) amends Section 1848 of the Social 7 Security Act (42 U.S.C. 1395w–4) and adds the following language:…”
…………..
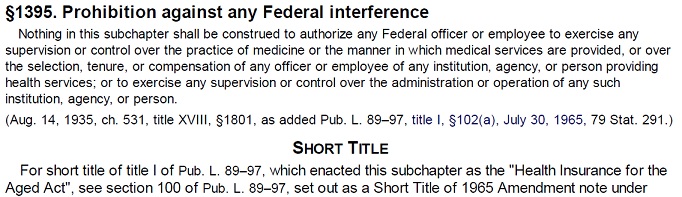
“The rules do not Improve physician payments and make payment to physicians harder to obtain for their services to patients. The rules impair the ability of physicians not only of maintaining a cost-effective practice, but of practicing medicine at all in the manner in which they see fit, especially in a private or small practice. This violates Section 1801 of the Health Insurance for the Aged Act that says “Nothing in this [subchapter] shall be construed to authorize any federal officer or employee to exercise any supervision or control over the practice of medicine, or the manner in which medical services are provided, or over the selection, tenure, or compensation of any officer, or employee, or any institution, agency or person providing health care services….” (Title 42, Section 1395, USC).
In addition, the rule harms access to care by Medicare patients by creating compliance protocols that are primarily based on cost of care and administrative factors. These rules specifically refer to a budget neutrality goal. The rule refers to withholding “incentives” from doctors who do not obtain arbitrarily defined budget and spending goals that can only amount to a rationing of medical care. Furthermore, physicians are coerced to comply with so called “quality measures” and are penalized for not obtaining arbitrary compliance thresholds set by the government and these rules. Such compliance fails to recognize the unique needs of individual patients, including those covered by Medicare. This amounts to a “one-size-fits-all (or most)” program that denies the specific medical care required by individual patients at different times in their lives based on the training, experience and judgment of the patient’s physicians. In addition, compliance with such measures has been specifically shown, in valid scientific studies, to directly injure or cause death to some patients and interfere in access to care for higher risk and other patients. Such programs do not increase access to Medicare, but decrease it, and these rules thus fail to comply with the law as proscribed by Congress.
We suggest modifying these rules substantially to address these and many other concerns. The MIPS program should not be implemented by the administration as currently envisioned by the proposed rules.
David McKalip, M.D.
Independent Neurological Surgeon
President, Florida Chapter of the Association of American Physicians and Surgeons”

Concise and excellent analysis and statement of the facts, imbedded contradictions, and ultimate nihilistic effects of MACRA.
I vote NO NO NO